VARICOSE veins, deep venous thrombosis, varicocele, and haemorrhoids are held here normally to be unequivocal manifestations of the saccharine disease, and also to exemplify in striking manner the value of the approach set out in Chapter I -- embracing the law of adaptation, and the distinction between, on the one hand, bodily defect and, on the other hand, personal make-up reacting with a new environmental factor. This contention was first put forward in 1950 [1] and later amplified in 1959 [2] and 1960, [3] and will now be summarized here.
I. Varicose Veins
-- The Prevailing View on the Causation, Held Here to be Untenable
Present-day medical opinion on the causation of varicose veins is very likely to blame the condition on an imperfect construction of the human body. Some conceive this imperfection to be an evolutionary one -- that is to say, the body is considered to be not yet properly adapted to its new upright posture, the veins of the leg being still insufficiently robust to support so long a column of blood. Others conceive the imperfection to be of the nature of a hereditary defect of the veins. In either case the body is considered to be built wrongly. It will be the aim of this chapter to contest this view and to substitute, instead, the view that the cause of varicose veins lies in the body being used wrongly.
This substitution can be achieved, it is submitted, partly by a consideration of the numerical incidence of varicose veins in Westernized countries, and partly by the differential incidence in civilized and uncivilized communities, on all of which we now have some highly relevant figures.
Taking first the numerical incidence, varicose veins at the present time occur to the extent of about 10 per cent in Westernized countries like Great Britain. [4] To suppose that the evolutionary forces, which during the adoption of the erect posture have modified man's arms, back, legs, and many other structures besides, should have failed also to have modified the leg veins is in itself difficult, but that they should have failed to the extent of 10 per cent is impossible, to believe -- representing as this figure does some 5 million sufferers in Great Britain and some 15 million in the United States. And even if these figures are modified later, the argument will still remain.
And as regards hereditary defects, usually presenting well-recognized characteristics and usually dating from birth (which varicose veins do not do), contrast the above incidence of 10 per cent, which is the same as 100 per 1000, with the incidence of congenital malformations, not one of which exceeds 5 per 1000 live births, as set out in Chapter I.
But the coup de grâce to the view that varicose veins are due to the body being built wrongly comes from the differential incidence of the condition in civilized and uncivilized communities. In this connexion we have valuable evidence from studies in the Negro. In the United States the incidence of varicose veins in both Negroes and whites is considered to be very much the same, whether in the great Charity Hospital in New Orleans [5] or the Cook County Hospital in Chicago. [6] It is true that today a minority of U.S. Negroes are of pure stock, [7] but if there were any congenital immunity to varicose veins in the Negro, it would be bound to alter the incidence away from that in the whites. Yet the evidence, as said, is that the incidence is very much the same.
Now contrast this incidence with that in the Negroes of Africa who are still living tribally, and who may therefore be regarded as still relatively uncivilized. In such Negroes it may be stated that for practical purposes neither varicose veins nor, for that matter, varicocele, are ever to be seen. Confirmation of this fact was given the author in 1958 in personal communications from Professor H. J. Croot and Mr. J. Cook, of Makerere College, Uganda; Mr. Anthony Barker, of the Charles Johnson Memorial Hospital, Nqutu, Zululand, Natal; Dr. J. D. B. Longley, Queen Elizabeth Hospital, Umuahia, Eastern Nigeria; Dr. D. C. Milton Thompson, Edwards Memorial Hospital, Mombasa; and Miss E. T. Mess, Wusasa Hospital, Northern Nigeria. Thus Professor H. J. Croot and Mr. J. Cook, in answering personal inquiries on the incidence of inguinal hernia, varicose veins, and varicocele in very primitive races, stated that fortunately they were able to help, because these three conditions were recognizable in field surveys carried out for leprosy and other infective diseases. For example, as regards inguinal hernia, they quoted figures by Dr. Kinnear Brown (1956), Government Leprologist, which gave an incidence of 0.69 per cent for this condition in the pygmy tribes of the Semliki Valley, Western Uganda, and 0.3 per cent in the very tall Karamojong tribe of Eastern Uganda. But as regards the other conditions, they stated that 'varicose veins and varicocele had never been noted in any of these tribal areas by any of the seven observers who have studied these peoples, and must be considered exceedingly uncommon'.
The author bestowed great labour in the past, including a personal visit to New Orleans in 1942, whilst passing through the United States, in elucidating the above commonness of varicose veins in U.S. Negroes, but their absence in tribal Africans, which distinction he regards as a crucial one in the present subject.
Later, in 1964, H. Dodd visited Africa to verify the latter assertions for himself, in natives still living tribally. The following is quoted from his subsequent paper in The Lancet. [8] 'I visited the Charles Johnson Memorial Hospital (600 beds), Nqutu, in the Zululand reserve. Ailments arising from infections, parasites, and nutritional imbalance are commonplace, but varicose veins are virtually not seen.
'Most of the patients (Zulus) lived tribally. The white medical staff, two of whom have worked there since 1945, confirmed the paucity of venous ailments. In January, 1964, Mr. Anthony Barker, the medical superintendent, reported that, in the previous three years, out of a total of 11,462 in-patient admissions (including 3141 maternity cases) and a total of 103,857 out-patient attendances, there were 3 patients with varicose veins, 1 pregnant woman with haemorrhoids, 3 with femoral thrombosis, and 3 patients with varicoceles.
'Although 4 patients had varicose veins of the vulva there was no instance of varicose veins in the legs of pregnant women. Femoral thrombosis followed parturition in the 3 women -- in 2 with fatal results.'
This evidence has been extended by A. Barker himself [9] to 5 cases of varicose veins in over 14,000 admissions.
The freedom from varicose veins, even in pregnancy, in these Negroes is of the deepest significance. It will also be noted, for future reference, that haemorrhoids and varicocele, both so commonplace in Western peoples as to vie in their incidence with that of varicose veins, are likewise almost completely absent.
But in contrast with these tribal Zulus, the urban Zulus, on a much more refined diet, as will be seen later, now show varicose veins and, for that matter, haemorrhoids, in fair numbers, so that the situation is approximating to that in the United States.
It may be added that the epidemiology of varicose veins and related venous ailments has recently been reviewed by Mr. Denis Burkitt [10] who supports the author's conclusions over these conditions, except for one or two differences which the author has not been able, himself, to accept [11] These conclusions are that the body is indeed not built wrongly, but is being used wrongly. The question is: In what manner is it being used wrongly?
II. Varicose Veins, Varicocele, Deep Venous Thrombosis, and Haemorrhoids
-- The View on the Causation Advanced Here
Now it is impossible to relate the vast difference in the incidence of varicose veins in the U.S. and African Negro to any difference in physical activity. The U.S. Negro even in the north probably works just as hard as his cousin works in Africa, and in the south he certainly does -- for what fundamental difference is there between toiling in the cotton fields in Louisiana and in the maize plantations of Natal? It must also be remembered that there is no appreciable difference between the incidence of varicose veins in the northern and southern U.S. Negroes, the incidence in each case equalling that in the whites. The argument now proceeds under separate headings, and it is assumed that obstructing the venous flow raises the pressure in the veins distally, causing them to become varicose, and likewise retards the blood flow in them, which is considered the basic cause of any clotting (thrombosis) that occurs.
1. Anatomical Considerations
To explain the above difference in incidence something much more crucial than physical activity must be invoked and a clue to the cause advanced here is given in textbooks of anatomy, [12] which sometimes ascribe the greater commonness of varicose veins in the left leg to the fact that at the brim of the pelvis the iliac part of the descending colon crosses over the left external iliac vein bringing up the blood from the left leg, and so the colon may partially obstruct the blood-flow from the leg (Fig. 3). Now if the author of this work has contributed anything to this subject, it has been to argue that, from the law of adaptation, the above anatomical relationship can never under natural conditions produce any venous obstruction whatever; but that in the presence of a refined, Westernized diet, bringing about unnatural loading of the colon, it can indeed produce such obstruction, and, in fact, becomes the fundamental cause of varicose veins.
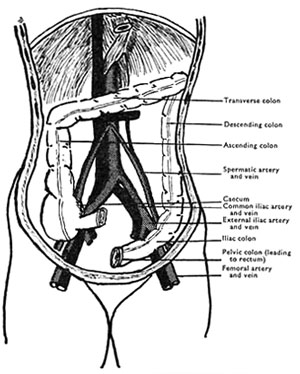
Fig. 3. -- The relationship of the colon to the arteries (cross-hatched) and veins (black) at the back of the abdomen (diagrammatic only). [3] (From an original drawing by Surgeon Commander R. Y. W. Lambert R.N.)
|
For, it must be added, it is not only the iliac colon that is related to the external iliac vein; on the right side the caecum is adjacent to the right external iliac vein, and if the caecum becomes distended as the result of colonic stases, it does not tend to rise upwards towards the liver but to fall downwards towards the pelvis, and so may cause a similar obstruction in the right vein. Indeed a prolapsed caecum is quite common, as surgeons who operate in this region know well.
It must be emphasized that there is no question of these parts of the colon floating freely in the abdomen, which would virtually preclude any local pressure on the external iliac veins. They have no mesentery (unless the caecum is prolapsed over the vein into the pelvis, when the question of a mesentery becomes relatively unimportant), but are in direct contact with the (external iliac) veins. Indeed R. J. Last, [13] in his work on anatomy (1966), describes the descending colon as 'plastered down' by the peritoneum. Moreover, the commencing pelvic meso-colon, which follows the line of the external iliac vein, but in an upward direction, is at first so short that the beginning of the pelvic colon is also closely applied to the vein. It may also be important that a loaded pelvic colon lower down could lead to a pulling across the vein, either by its direct continuity with the iliac colon or by its mesentery, [14] just described; indeed some may prefer this alternative view. It must always be remembered that the resting pressure of blood in the iliac vein is only a few millimetres of mercury. For this same reason the intervention of the external iliac artery, in which the pressure of blood is vastly higher, would offer no protection, as any colonic pressure would be at once transmitted through it to the vein.
2. Significance of Preponderances in the Left Leg
To look more closely into this question of the relative incidence of varicose veins on the two sides of the body, it is clear that in the erect position, since the iliac veins are running almost vertically downwards, any positional superiority of the left colon over the caecum, in being able to obstruct the vein, will be small, but that in the supine position, since the left colon will still be crossing over the vein, whereas the caecum on the right may be falling away from the vein, laterally, this superiority of the left colon will become considerably magnified. It is consistent with these facts that the incidence of varicose veins is only about 10 per cent greater on the left side, [15] whereas the clinical incidence of ileofemoral thrombosis, in many references, is nearly three times greater on the left side, as shown in Table II.
Table II -- Incidence of Ileofemoral Venous Thrombosis on the Two Sides,
According to Various Observers
|
| Date |
Author
|
Total Cases
|
Percentage
Incidence
on Left
|
Percentage Incidence
on Right
|
Bilateral
|
| 1784 |
White [16] |
9
|
65
|
35
|
|
| 1938 |
Atkins [17] |
34
|
82
|
9
|
9
|
| 1940 |
Barker [18] |
210
|
72
|
28
|
|
| 1943 |
Ehrich and Krumbhaar [19] |
16
|
50
|
18.7
|
31.3
|
| 1967 |
Negus [20] |
88
|
53.5
|
27
|
19.5
|
| 1967 |
Cockett, Lea, Thomas and Negus [21] |
57
|
70
|
30
|
|
| 1967 |
Mavor and Galloway [22] |
38
|
75.3
|
24.7
|
|
For varicose veins occur chiefly in people who are up and about for most of the day, though they are recumbent at night. But ileofemoral thrombosis occurs predominantly in bed-patients, whether due to illness, childbirth ('white leg'), or following operation, the patient thus being nearly always in the supine position.
The significance of the figures in Table II is not lessened by the fact that fibrinogen and other tests often show thrombosis to be present on both sides. For quite apart from thrombosis beginning during the trauma of certain (especially pelvic) operations, to be mentioned later, Doran and others [23] have shown that during any major operation the venous return is always slowed by a half, and not infrequently slowed to the level found in a paralysed limb, so no doubt nuclei of thrombosis often do form on both sides (for Virchow showed long ago how important slowing is in the causation of thrombosis). But whether these nuclei increase in number, expand, and coalesce until the state of clinical thrombosis is reached, often around the tenth day and with or without pulmonary embolism, depends on an added factor, which the present author believes to be the unnatural loading of the colon, described above. Therefore, to him the clinical thrombosis is what is of paramount importance, and it is the great preponderance of this clinical thrombosis on the left side that is so revealing and that points to the prophylaxis shortly to be advanced. On this line of reasoning fibrinogen-testing soon after operation, recently described as largely impracticable [24] in any case, seems often to be irrelevant.
(It must be added parenthetically at this juncture that very similar reasoning to the foregoing can explain the causation of varicocele, which in the vast majority of cases is confined to the left side, since on this side the iliac colon crosses directly over the left spermatic vein, whereas on the right side the caecum does not cross over the right spermatic vein, and in addition is partly kept away from it by the larger mass of the external iliac vessels.)
As regards the argument sometimes heard, that with an unrefined diet the extra bulk of the colonic contents would lead to greater, not smaller, pressures on the iliac veins, the following considerations must be borne in mind, as the author has set out elsewhere. [25]
- The complex hydrodynamic factors within the abdominal walls would preclude this being the case, however voluminous the colonic contents, unless the specific gravity of these contents were sufficiently raised above that of the peritoneal fluid, which, for evolutionary reasons, would be unlikely to occur except in the presence of unnatural stasis (and consequent accumulation of intestinal sand, which forms a considerable proportion of these contents). And it is to be noted that the behaviour of a stool in water is an unreliable guide in this respect, because any trapped gases of intestinal fermentation in the stool could lead to its floating when otherwise it would sink.
- The extra bulk arising from the diet is held here to be more than compensated by the much faster transit time. In this respect the author is privileged to quote the following personal communication (dated 10 September, 1972) from Mr. Anthony Barker, who has provided much vital information on this subject from Africans living tribally, as seen above and elsewhere in this work.
'... The Zulus do have more frequent and more bulky stools than do the whites of England, but the crucial point is that their transit times are much more rapid, averaging only 24 to 36 hours. In answer to your question about findings at operation, a loaded colon is quite exceptional in these people.'
- Finally, there is the actual sensation of colonic well-being so familiar to people having a natural consumption of fibre and consequently a fast intestinal transit time. To suggest to those who clearly recognize this definite sensation that it is based on colonic loading, instead of colonic emptiness, would be met with astonishment; and palpation of the abdomen would rapidly settle the matter.
3. The Rising Incidence of Pulmonary Embolism and Deep Venous Thrombosis in the Legs
It is vital to the argument now being presented that the incidence of pulmonary embolism, most of which is due to deep-leg thrombosis, has been rising very markedly in this country in recent years. A crucial paper by Morrell, Truelove, and Barr, [26] working in the Radcliffe Infirmary and Churchill Hospital, Oxford, shows that the incidence of this condition increased approximately fivefold in the decade 1952-61, and that though about a third of these cases were postoperative, the remainder were medical bed-patients, who had had no operation at all (thus suggesting that what is concerned in this rise may be something quite independent of an operation itself). These authors also quote European studies showing results not inconsistent with their own, with the frequency of pulmonary embolism and leg thrombosis decreasing during, and immediately after, each World War, but always recovering later, to resume a steady upward trend.
This rising incidence of pulmonary embolism and leg thrombosis is perfectly in accord with the general causation put forward here -- the ever-increasing consumption of refined carbohydrates in Westernized countries, which has culminated in present transit times of the bowel contents now being about twice as long as the natural transit times (see Chapter III). But what is so instructive is that during the period now under consideration there has been a special aggravation of this cause, which will now be set out and which will be seen greatly to strengthen the whole of the present argument. Perhaps slightly because of the shortage of nurses and the shortening of their hours of work, this aggravation has consisted in the shading off, or even open abandonment, some 20 years ago, of various hospital preoperative purgative and enema routines, except for special operations, as on the bowel. It was Mr. Conrad Latto who first spoke to the author of this change in surgical practice during the 1950's, which came in gradually and to varying extents in different localities, and the same thing was confirmed by the late Mr. A. Elliot-Smith (of the Radcliffe Infirmary), Mr. L. Knights, and others, including Surgeon Vice-Admiral J. Watt, who consulted senior naval nursing staff on this point. There seems no doubt that this change has commonly occurred during the 1950's, and its possible relevance (on the argument at present being advanced) to the big increase in pulmonary embolism and leg thrombosis over much the same period, described above, is obvious. It is to be noted, too, that the frequent substitution of suppositories for enemas, which seems to be another labour-saving change of the same type that has taken place, would also have an unfavourable effect with regard to the removal of any high accumulations, such as those present in the vital iliac colon, and even higher.
And now, with regard to the realities of the colonic stasis at present being discussed, the author would like to make two quotations. The first is taken from Mr. Harold Dodd's foreword to the author's early monograph on varicose veins, now largely superseded by the present volume: 'It is my practice to teach that patients confined to bed seldom empty the colon; even if they have a daily action, it is merely an overflow. I have been impressed with this again and again when operating ... their bowels are often laden with plastic faeces from the caecum to the rectum.' Loading of the iliac and lower colon is of course well recognized, as inquiries of many surgeons have confirmed, and the author would add that he has, himself, on countless occasions rolled a loaded iliac colon under the hand on ordinary clinical palpation of the abdomen, as other physicians will remember doing, too.
The second quotation is from a much less distinguished source, but, considering the seriousness of the present situation over leg thrombosis, the author thinks that such a clear and absolutely disinterested observation is well worth reproduction, and that where the truth is so pressing,
'One glimpse of it within the Tavern caught,
Better than in the Temple lost outright.'
Thus I refer to Dr. John Rowan Wilson's (nom de plume for the late Dr. John Robinson Wilson) contribution to the medical columns of The Spectator on 24 August, 1970:
'A friend of mine recently went into hospital for the treatment of depression. She had been admitted for the same condition a number of years ago, and she was fascinated to see how everything had changed. In the old days the emphasis was all on spit and polish and the traditional nursing routine. Patients were awakened at six o'clock in the morning, beds had to be neat and tidy, temperature and pulse were religiously charted. Sister was obsessive about bowel movements: if anyone missed a day it was big news; aperients and enemas were immediately enlisted to bring her up to scratch.
'After a ten years' interval the atmosphere was unrecognizable. It was cheerful, chatty and informal. The emphasis was not on physical treatment but on making the patient feel at home and allowing her some freedom to express herself. The nurses were far more interested in home backgrounds and troubles with husbands and children than with temperature charts and bowel movements. Most important of all, patients were encouraged to form a mutually supportive community. They spent most of their time talking to each other. "And what did they talk about?" I asked my friend. "Their bowels, mostly", she said. "They were all as constipated as hell." '
4. Straining at Stool not considered here the Key Factor
Apart from the special instance of haemorrhoids (where a particular muscle-factor is involved, as shown in Fig. 4), the author, himself, cannot accept, what has several times been suggested to him, that straining at stool is of any great significance in the aetiology of varicose veins or deep venous thrombosis. For one thing, if straining were aetiologically important, venous ills would be expected to be prominent in patients with chronic cough, which is definitely not the case. Furthermore, it is quite unnecessary to postulate any such high venous pressures in the aetiology. What is much more deadly than a temporary high pressure, that is to some extent natural and adapted to, is a long-continued low pressure that is not natural and not adapted to. Thus a series of long jumps, or a cross-country run, inflicts enormous strain on the spring ligament supporting the arch of the foot, but normally leaves it unscathed, whereas the unnatural constant strain of even a stone of overweight can flatten it right out. This 'inevitability of gradualness' is also seen in the case of the tiny but long-continued forces of the starfish eventually breaking down the vastly greater but less sustained forces of the oyster, which is thus opened and devoured. It is not wise to minimize the unnatural and continual back-pressure effect on the valves of a vein, that must result from a loaded colon lying across the vein, which back-pressure the valves are not evolved to support, and due to which they tend to dilate and become incompetent.
Stemming from the above it has even been suggested that the squatting position at stool, by reducing the effects of straining, explains the lack of venous ills in tribal Africans, referred to earlier. But anyone who tries an unrefined diet knows that with such a diet the call to stool is so urgent that no straining worth discussion is possible in any case, but that, per contra, with a refined diet the straining can be very severe no matter what position is adopted. All this quite apart from the fact that some crouching is instinctively adopted, anyway, even at the height which has been found most convenient for the construction of closet seats. What is needed in Westernized countries today is not the reconstruction of millions of these seats, but the restoration to the diet of the fibre of which it has been robbed.
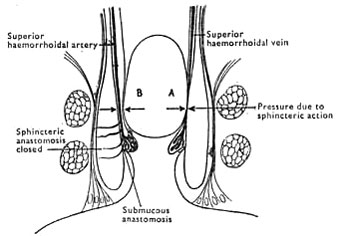 Fig. 4. -- A, Superior haemorrhoidal vein compressed between the contracted sphincter and a hard faecal mass. B, Superior haemorrhoidal artery unaffected by compression and continuing to supply blood to the venous plexus. (Reproduced with permission of the publisher from A. G. Parks.) [35]
Fig. 4. -- A, Superior haemorrhoidal vein compressed between the contracted sphincter and a hard faecal mass. B, Superior haemorrhoidal artery unaffected by compression and continuing to supply blood to the venous plexus. (Reproduced with permission of the publisher from A. G. Parks.) [35]
|
With further regard to straining at stool, it has been postulated that past straining, through having damaged the venous valves, is the essential cause of postoperative thrombosis. Quite apart from the failure of this postulate to explain the striking clinical preponderance on the left side, already alluded to, a strong additional reason can be advanced against it. For if past straining were the essential cause, then any operation cases with varicose veins (themselves constituting the best evidence of past damage to the valves) would be expected to suffer from postoperative thrombosis decidedly more often than operation cases without varicose veins. Yet Kemble [27] has recently shown in a survey of 280 cases at the Middlesex Hospital that there was no difference in postoperative thrombosis between the two groups. The fact is that in the supine position, where the blood is flowing horizontally, the valves in the veins are hardly being used at all and so their integrity is relatively unimportant (which is, of course, why varicose ulcers heal up in this position). But be it noted that, in sharp contrast to the above, the result of this Middlesex survey is in no way harmful to the view that the causation of most postoperative thrombosis lies in unnatural colonic loading, for such pressures will slow the blood flow in the external iliac veins, whatever the state of the valves below.
There must also be considered the question of varicose veins in pregnancy. It is established that these normally appear early in pregnancy, when the fetus is too small to be able to exert any pressure on the veins. (This, quite apart from the fact that evolution must have ensured that no such pressure shall occur anyway.) Now it is well known that a severe constipation is likely to occur early in pregnancy, precipitated by the common occurrence of morning vomiting at this time, which interferes with the food intake. It is thus easy to relate the varicose veins to the pressure of a loaded colon but not to straining at stool, for they usually disappear after the pregnancy is over, which any stretched valves of the veins would not allow (the valves being fibrous in structure).
It is also important to add to the foregoing that the attribution of venous ills to straining at stool, instead of to direct colonic pressure on the iliac veins, would be a very serious thing as regards therapeutics. For postoperative leg thrombosis often cannot be due to present straining at stool since the thrombosis often happens before any such straining is possible. So prophylaxis would often be impossible, too. Whereas, if direct colonic pressure is the cause, prophylactic attention to the state of the bowel, as will shortly be described, becomes not only of crucial importance but also perfectly feasible.
5. The Question of an 'Iliac Compression Syndrome'
We must now pause to examine other theories of causation of the venous ills we have been discussing. To explain the big difference in the incidence of femoral thrombosis on the two sides Aschoff [28] and others, who regard recumbency as the dominant cause of most femoral thrombosis, have contended that the reason lies in the right common iliac artery crossing over the left common iliac vein, and Williams [29] has even implicated this normal anatomical relationship in the production of varicose veins themselves. Meanwhile, to explain the even bigger difference in the incidence of varicocele on the two sides, most textbooks of surgery give the fact that the left spermatic vein opens into the left renal vein at right-angles, without a valve, whereas the right spermatic vein opens into the vena cava obliquely, with a valve. But both the above explanations are completely incompatible with the law of adaptation, as set out in Chapter I, and furthermore each of the explanations is rendered weaker by the existence of the other. For it would be a coincidence indeed if evolutionary errors occurred in both the right iliac artery and the left spermatic vein. In that case the body would be expected to be full of errors, whereas the figures for hereditary defects in Chapter I show just how rare evolutionary errors are -- and moreover they are not errors in mechanical conception.
In connexion with the foregoing, we must take note of a more recent elaboration of the first of these postulated anatomical causes. F. Cockett and others, also seizing on the marked preponderance of ileofemoral thrombosis on the left side, likewise incriminate the right common iliac artery crossing the left common iliac vein 'as the main aetiological factor' in the production of the thrombosis, and have advanced radiological and post-mortem findings in support of such a mechanism, under the title of 'The Iliac Compression Syndrome'. [30]
For those, however, who steadfastly refuse to blame the evolutionary adaptation of the human body, but who look instead for an unnatural factor in the environment, as the cause of the present troubles, this view presents no terrors. In the first place the phlebograms, and the denting of, and adhesions inside, the vein opposite the crossing, which these writers have found in 14 out of 100 cadavers, do not include any comparable studies in populations who do not suffer from these venous ills, such as the tribal Africans mentioned above. If the findings in these subjects proved to be much the same as in Westernized ones, such findings would emerge as not of pathological significance. But if such findings were absent, there is an explanation for their presence in Westernized subjects, which is not in conflict with human evolution. This is that in Westernized subjects, in whom these venous ills abound, the crossing of an unnaturally loaded colon over the lower iliac vein, through interfering, however slightly, over many years with the venous pressures in the vein above this crossing, leads to the very effects of the artery on the vein which the writers describe.
Meanwhile, in order to explain the cases of deep thrombosis in the right leg, which in the present book is related to stasis in the caecum, the above writers incriminate yet another artery -- the right external iliac artery pressing on the right external iliac vein. Lastly, the compression syndrome cannot explain the very big preponderance of varicocele on the left side, which a colonic cause can do.
In the second place, the 'iliac compression syndrome' cannot explain the great increase in deep leg thrombosis that has occurred over the past 20 years, as has already been set out here.
Finally, there is a third and subtler consideration that can be advanced against this syndrome, which may be expressed as follows: if the left hand encircles with moderate pressure the right wrist, and if the right hand is then (a) hung downwards and (b) repeatedly clenched, it is obvious that the veins of the hand will at once become prominent. Similarly, any arterial compression effect on the left iliac vein, as described in the above syndrome, would become far more noticeable when the subject was erect and at exercise than when he was lying down and at rest. Therefore varicose veins, which are commonly seen in people who are up and about, would be expected to have a much greater left-sided preponderance than would deep leg thrombosis, which is so often associated with recumbency. Yet in reality the exact opposite occurs (which, however, accords perfectly with a colonic cause, as already shown).
That the above anatomical sites, and Poupart's ligament too, form natural areas of arrest in cases of spreading thrombosis is not contested for a moment, but this leaves the reason why the thromboses occur in the first place unsolved, and the crucial difference between the above postulate and the one advanced here is that the latter leads to vital possibilities in prevention. For if the natural artery-pressure were basically implicated in the causation of deep leg thrombosis, such pressure could not normally be removed and so no prevention could be undertaken. But if a colon, unnaturally loaded through the diet of Western civilization, is basically implicated, prevention becomes immediately possible. This would consist ideally in restoring the natural fibre to the diet by taking substances such as the unprocessed bran described in Chapter III, so that the natural transit time of approximately 1-1/2 days (Chapter III) replaced the present 3-5 days seen in Westernized societies. If this restoration were not feasible, suitable bland aperients would be needed, with or without enemas as necessary. Such steps would be important in medical bed-patients, and also in confinement and operation cases (where the restoration of the natural transit time, if possible before the event, would in the opinion of the present writer bring about a rapid reversal in the climbing incidence of leg thrombosis). There would in these latter cases then be no need for the present extremely early getting-up after operation, which, as in the case of leg exercises, has signally failed to prevent the quadrupling of the incidence already referred to. It is, however, fully realized that a considerable number of thromboses are due to inevitable direct trauma to the iliac veins in certain (especially pelvic) operations, which cases may obviously need further measures, such as heparin, etc.
It is also clear, from the cause advanced here, that, as regards deep thrombosis, a prone position of the patient is far safer than a supine one, since in the former position no colonic accumulations can press on the (iliac) veins in any case, and indeed it is fair to point out that the very fact that this position has been found so beneficial [31] in practice is itself in favour of the correctness of this cause.
Finally, as regards the frequent earlier implication of the deep calf veins than the iliac and femoral veins in the thrombotic process, there is no reason why the repository of the back-pressures described above should not first be more evident in the more peripheral veins than in the more central ones.
Further to all the above, it has been recently demonstrated [32, 33] that increasing the blood-flow in the lower limbs during operation, by intermittent compression with inflatable splints, is 'a potent prophylactic against postoperative deep vein thrombosis'. This evidence dovetails perfectly with the prophylactic step advanced here, of preventing any impediment to the blood-flow from pressure on the veins by a loaded colon.
6. Prophylaxis of Deep Venous Thrombosis
Amongst those who have put whole surgical wards on to unprocessed bran, in an effort to reduce the incidence of postoperative thrombosis, on the argument just set out, are Mr. Conrad Latto of the Royal Berkshire Hospital, Reading, and Surgeon-Commander N. J. Blacklock of the Royal Naval Hospital, Haslar. Both have been immeasurably helped by the complete conviction, and from this the complete co-operation, of the sister in charge of the ward, which, in the author's experience, is without question the most important factor of all in success. Mr. Latto [34] has already reported excellent results with these patients as regards the behaviour of the bowel, resulting in the elimination of aperients from the ward, and Surgeon-Commander Blacklock has confirmed this finding in a personal communication to the author. As regards the occurrence of postoperative thrombosis, it is clear that single-ward experience can never become more than a pointer, encouraging others to carry out a comprehensive trial. With this absolute proviso, Mr. Latto writes (March, 1973): 'We have had no case of postoperative thrombosis in this ward for over 18 months. One case of thrombosis was admitted from outside and had a fatal embolism -- and it may be added that at post mortem the left colon was solid with hardened faeces.' Surgeon-Commander Blacklock's experience to date is similar in that 'We have had only one case of postoperative thrombosis in a little over one year, and this occurred in a man who had established congestive cardiac failure, which was presumed to be the basic cause in this case.' Eight months later (November, 1973) these favourable results continue, and recently Mr. Maurice Frohn has introduced the taking of unprocessed bran into his surgical wards at the Bethnal Green Hospital, London, in an effort to prevent postoperative thrombosis. The author is confident that Mr. Frohn will have much to contribute to this form of prophylaxis, especially in gastro-intestinal operations.
Finally, it must once again be emphasized how much everything depends on the co-operation of the ward sister. Thus, Mr. Latto's patients are given three tablespoonfuls of bran and are allowed to get it down as they please during the day -- in milk, soup, water, etc. In Surgeon-Commander Blacklock's patients the bran is taken along with the meals, or mixed in with tomato juice, in which it has been found most palatable and easy to take. It is the ward sister who will ensure that operation cases have no accumulations in the rectum, either by the taking of the bran or, if there has not yet been time for this to work, by clearance enemas.
7. Haemorrhoids
With regard to haemorrhoids, their causation is held here to be due to a very similar mechanism to that involved in the production of varicose veins and varicocele, the only difference being that in this case the pressure of faecal accumulation is exerted on veins within the bowel instead of on veins without. This pressure effect is greatly aggravated by straining at stool, in the effort to pass the constipated motion (see Fig. 4). It must be added that constipation as an important factor in the causation of haemorrhoids has long been recognized.
8. Further Considerations
As regards another condition mentioned earlier, an added note may be made on the tendency for varicocele to become much less conspicuous as age advances. In the author's opinion this may lie in young people, as they grow older, getting tired of the waste of time and effort caused by constipation and gradually joining the army of 7 million regular aperient-takers in this country, already referred to in the last chapter.
It is also worth pointing out that, in the absence of obvious pressure causes, such as tumours, or cirrhosis of the liver, no clinical varicosities occur in the human body except where obstruction due to colonic stasis can account for them. Indeed, this peculiar localized distribution of clinical varicosities in the body weighs heavily against any postulated general cause of such varicosities -- such as, for example, some blood condition. And for this reason any attack on postoperative thrombosis by injections of heparin, etc., however expedient this may appear, must -- as long as a basic cause is not removed -- always savour of two wrongs not making a right. This at least is the opinion of the present writer, holding the view on the causation that he does.
* * *
To turn back, it now becomes possible to see very clearly why there is so great a difference in the incidence of all these venous obstructions in the two groups of Negroes which were referred to. For the Negroes in the United States are eating the same refined carbohydrates as are the whites, whereas those living tribally in Africa are subsisting on a diet almost wholly composed of crudely ground maize or other unrefined carbohydrates. The very large quantity of fibre ingested by the tribal Africans has a striking effect on the quantity and the quality of the stools. These are passed twice a day and are extended like a ribbon of toothpaste some 15 in. long, and of the diameter of the middle finger. They are in fact known locally as the 'toothpaste stool'.
In this connexion it is important to point out that the rate of passage of the colonic contents cannot be assessed by the regularity of the motions passed. These may be passed with the utmost regularity -- but may always be one day late! The rate of passage can, in fact, only be assessed by the consistency and diameter of the motion. If the rate is the natural one, i.e., if there is no unnatural stasis present, the consistency will always be soft and the diameter not appreciably greater than that of the middle finger.
The reality of colonic stasis in Westernized countries is revealed by the enormous consumption of aperients in these countries, as shown by the M. R.C. research workers' figures set out in Chapter III. The reality of the stasis is likewise revealed by the dramatic change in the rate of passage of the colonic contents produced by restoring to the diet the fibre removed in the refining of flour, as in the taking of unprocessed bran described in the diet card at the end of this volume and referred to in Chapter III.
III. Personal Build and Heredity, in the Production of Varicose Veins
There are few more pronounced examples in the body, of differences in personal build, than occur in the human colon, which varies greatly, not only in its general position, but also in the length of its mesenteries. Consequently there is great scope in some colons, when unnaturally loaded, for pressing on the iliac veins, whereas in others there is no scope at all. Therefore, on a diet containing refined carbohydrates some persons will develop varicose veins and some will not. But, let it be noted, on a diet of unrefined carbohydrates, with no colonic stasis, no persons will develop varicose veins, no matter what the build of their colons.
Exactly the same type of argument applies to the occurrence, in the presence of a refined diet, of varicocele in some persons but not in others. And likewise to the occurrence of haemorrhoids. As regards haemorrhoids, it has been known for a very long time that colonic stasis in some persons is centred in the rectum itself. In fact over 30 years ago Arthur Hurst introduced the term 'dyschezia' for just this form of constipation. It is therefore easy to understand why, though these venous conditions (e.g., varicose veins and haemorrhoids) do have a tendency to occur together, they very frequently occur separately.
* * *
Finally, it will now be seen that, against the above background, the question of heredity is of no practical importance, because, as stated in Chapter I, it is just as easy to inherit personal build as bodily defect. Therefore, the presence of any hereditary element in varicose veins, varicocele, or haemorrhoids does not alter the fundamental situation one iota, nor our approach to it as regards treatment. Any preoccupation with heredity, in fact, would, as stated in the earlier chapter, be a case of drawing a red herring across the trail.
IV. The New Indications in the Prevention and Arrest of Varicose Veins, Varicocele, and Haemorrhoids
The author would be the first to agree that the evolutionary and racial evidence for the view advanced here, on the causation of these venous conditions, needs the added support of direct experimental studies, involving barium meals and other devices; and indeed it is his ambition to initiate such studies in the future. He would like, for example, to see what proportion of people with well-marked varicose veins in the right leg, or with a right varicose ulcer, have a prolapsed caecum, compared with people without these conditions. Such cases as Mr. Conrad Latto and other friends have looked into for the author, via barium meals, have for the most part shown partial or complete prolapse of the caecum, though even a normally placed caecum, if distended, could edge over onto the external iliac vein. Very recently a complete absence of gravitational ulcer has been reported in 9000 Iranian patients examined in Iran [36] -- and their food was unrefined wheat and unrefined barley. Clearly all this points to a hopeful approach in treatment for the unfortunate sufferers from leg ulcer.
Believing as the author does, then, in the view advanced here, and unless experimental studies destroy it, he considers the essential step to be taken in all these venous conditions is the same substitution of unrefined carbohydrates for the refined ones -- that is to say, basically, the substitution of raw and dried fruits for sugar, and sweetstuffs, etc., that contain sugar; and of a true wholemeal bread for white bread and all confectionery, etc., containing white flour. But no other dietetic steps are needed, and no harsh régime is therefore in question.
The above dietetic substitution will itself have a profound effect on the action of the colon, but if the stools do not change adequately to the natural form described above, the process can easily be completed by the taking of a little unprocessed bran each day, as set out in the card mentioned.
The above steps effectively remove the cause of all three of the venous conditions now under consideration. This may be sufficient treatment of itself in the early stages of the conditions, but of course local treatment will obviously be indicated, also, in the later stages -- just as the same diet will prevent and arrest dental disease, but will not save a tooth from needing local treatment once a certain stage in the disease-process has been reached.
Local treatment, however, must never displace the removal of the cause. This is well seen in the case of postoperative femoral thrombosis and pulmonary embolism, the incidence of which, in spite of all the leg exercises, breathing exercises, and early ambulations, has, as already stated, nearly quadrupled in recent years. No one who understands the argument set out here, and who gives a glance at the foods eaten in the ordinary hospital, will share in the general perplexity occasioned by this increase.
Furthermore, quite apart from the question of persistence and recurrence, one of the decisive advantages in the conception of a single saccharine disease is the futility revealed of trying to 'get away with' the surgical treatment of one of the manifestations of the disease without simultaneous permanent removal of the cause, by the dietetic steps indicated above. For unless this removal of the cause is instituted, the patient remains completely exposed to one of the other manifestations. For example, where is the profit in having, per se, a haemorrhoid injected, if later all the teeth are to be lost from pyorrhoea? Better to keep the haemorrhoid, if it forces a dietetic reform. Otherwise, it is submitted that this would be another case of trying to be clever at Nature's expense.
References
1. Cleave, T. L. (1956), J. R. Nav. Med. Serv., 42, No. 2, 550.
2. -- (1959), Lancet, 2, 172.
3. -- (1960), On the Causation of Varicose Veins. Bristol: Wright. (U.S.A.: Williams & Wilkins Co., Baltimore.)
4. Foote, R. R. (1952), Varicose Veins, 2nd ed., 38. London: Butterworths.
5. Menendez, C. (1960), personal communication quoted in reference 3.
6. Kozoll, D. (1963), personal communication, quoted in Cleave, T. L., and Campbell, G. D. (1966), Diabetes, Coronary Thrombosis, and the Saccharine Disease, 1st ed. Bristol: Wright.
7. Lewis, J. H. (1942), The Biology of the Negro. Chicago: University Press of Chicago.
8. Dodd, H. (1964), Lancet, 2, 809.
9. Barker, A. (1964), Lancet., 2, 970.
10. Burkitt, D. P. (1972), Brit. Med. J., 2, 556.
11. Cleave, T. L. (1972), Ibid., 3, 177.
12. Brash, J. C. (1948), Cunningham's Manual of Practical Anatomy, 11th ed., 2309. London: Oxford University Press.
13. Last, R. J. (1966), Anatomy, Regional and Applied, 4th ed., 401. London: Churchill.
14. Cunningham's Manual of Practical Anatomy (1937), 9th ed., 325. London: Churchill.
15. Weddell, J. M. (1969), Brit. J. Prev. Soc. Med., 23, 179.
16. White, C. (1784), quoted in Negus, D. (1970), Ann. R. Coll. Surg. Engl., 47, 92.
17. Atkins, H. J. B. (1938), Guy's Hospital Reports, 18, 92.
18. Barker, N. W., Nygaard, K. K., Walters, W., and Priestley, J. T. (1940), Mayo Clin. Prac., 16, 33,
19. Ehrich, W. E., and Krumbhaar, E. B. (1943), Amer. Heart J., 26, 737.
20. Negus, D. (1970), Ann. R. Coll. Surg. Engl., 47, 92
21. Cockett, F. B., Lea Thomas, M., and Negus, D. (1967), Brit. Med. J., 2, 114.
22. Mavor, G. E., and Galloway, J. M. D. (1967), Brit. J. Surg., 54, 1019.
23. Doran, F. S. A., Drury, M., and Sivyer, A. (1964), Ibid., 51, 486.
24. -- (1973), Brit. Med. J., 2, 612.
25. Cleave, T. L. (1972), Ibid., 4, 612.
26. Morrell, M. T., Truelove, S. C., and Barr, A. (1963), Ibid., 4, 830.
27. Kemble, J. V. H. (1971), Brit. J. of Hosp. Medicine, 6, No. 6, 726.
28. Aschoff, L. (1924), Lectures on Pathology, 253. New York: Paul B. Hoeber.
29. Williams, T. H. (1959), Lancet, 1, 1010.
30. Cockett, F. B., Lea Thomas, M., and Negus, D. (1967), Brit. Med. J., 2, 14.
31. Osborn, D. M., and Osborn, G. R. (1965), Lancet, 1, 983.
32. Sabri, S., Roberts, V. C., and Cotton, L. T. (1971), Brit. Med. J., 4, 394.
33. Hills, N. H., Pflug, J. J., Jeyasingh, K., Boardman, L., and Calnan, J. S. (1972), Ibid., 1, 131.
34. Latto, C. (1972), Ibid., 3, 705.
35. Parks, A. G. (1956), Brit. J. Surg., 43, 337.
36. Griffiths, W. A. D. (1972), Brit. Med. J., 2, 770.
Next chapter
Table of Contents
Back to the Small Farms Library Index

Community development | Rural development
City farms | Organic gardening | Composting | Small farms | Biofuel | Solar box cookers
Trees, soil and water | Seeds of the world | Appropriate technology | Project vehicles
Home | What people are saying about us | About Handmade Projects
Projects | Internet | Schools projects | Sitemap | Site Search | Donations | Contact us